Written by: Yusof Hassan
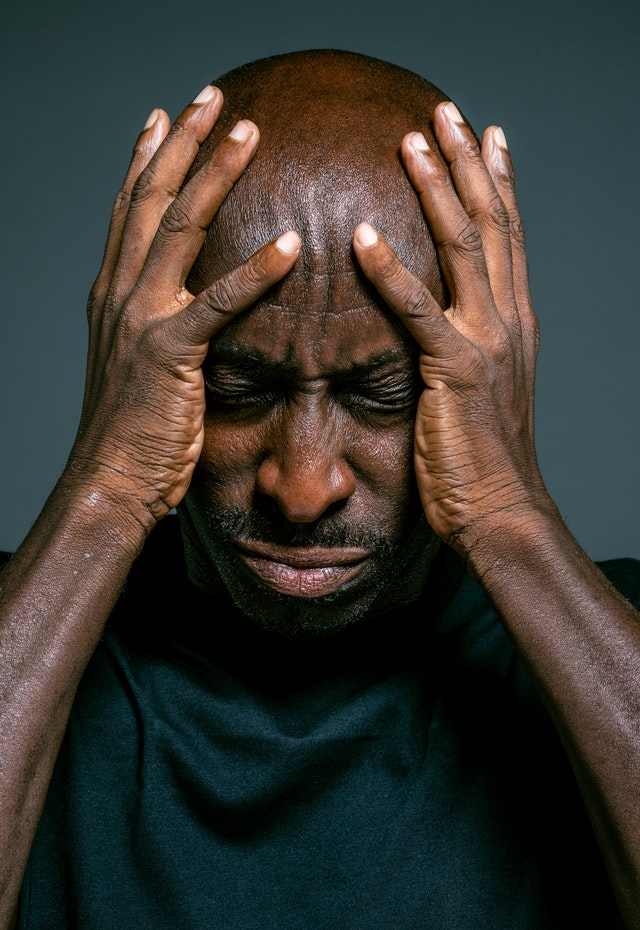
In many communities, mental illnesses are rarely spoken about, and so can go under the radar until causing real issues. With the ongoing COVID-19 pandemic, mental health issues have been on the rise.
The Mental Health Foundation has identified factors that affect BAME communities’ mental health that don’t affect their white counterparts, including racism/discrimination, social and economic inequalities, and the criminal justice system, among other factors (“Black, Asian and Minority Ethnic (BAME) Communities” 2015). From previous articles, we have examined how and why BAME communities may experience more significant mental health problems than most in the UK. Therefore, this issue is incredibly important to make aware of in African communities.
However, studies show that, specifically in African communities, these mental health issues are quick to be overlooked. A qualitative study by BMJ journal (Memon et al. 2016) concludes that there is a lack of sufficient information and awareness about mental health issues in BAME backgrounds. This introduces the dangerous stigma surrounding mental illnesses in African communities that can cause further damage.
Why is mental health stigma a serious issue? Stigma can cause delays, or even dismissals, of people suffering from these illnesses from attending therapy. In communities where mental health is not taken seriously or even seen negatively, those suffering from it will not take up professional help. Therefore, they can end up spiralling down, both emotionally and physically, which can further affect financial positions through a lack of optimal working, among other things.
The question of where this stigma comes from is yet to be solidly answered, although there are many different factors that could play into it. It is important to note first, that although this is specified at BAME, and specifically African, communities, this doesn’t ignore the stigma in White British communities, nor does it excuse White Britons from making the same mistakes associated with these problems.
Nevertheless, when analysing this problem in African communities, one of the many schools of thought surrounding stigma is employment opportunities. A previous article broadly paints a picture of a common mindset that is adopted by non-British workers and their families, aptly named the Immigrant Mentality. Although the generic term definitely isn’t applicable for everyone in BAME communities, it does stress the importance of work in the overall BAME communities’ view. Consequently, stigma can arise as admitting one or someone in one’s family has mental health issues can spark concern and worry that this will affect their ability to gain employment in the economy.
A research GAIN paper about African communities in Nottingham hints at this problem. The data in it shows that the two greatest needs of African community members are academic study (18%) and employment (11%), while emotional/psychological needs were only 3.1% of the community’s answers. This signals that mental wellbeing is severely undervalued in Nottingham African communities.
As these issues have evidently affected communities disproportionately, with BAME communities receiving the worst of it, this stigma must be abolished as quickly as possible, so that those affected by mental health problems get the attention they require, and therefore strengthen African communities in total.
There are many places to look for help to do with mental health issues, including another GAIN article here. Spreading awareness of this as a serious issue is something that must be done, through government information provision, charity work like that being done by GAIN, and personally, by speaking to your family members and friends about being open and accepting toward these difficult issues.
Sources- “Black, Asian and Minority Ethnic (BAME) Communities.” 2015. Mental Health Foundation. August 7, 2015. https://www.mentalhealth.org.uk/a-to-z/b/black-asian-and-minority-ethnic-bame-communities.
Memon, Anjum, Katie Taylor, Lisa M Mohebati, Josefin Sundin, Max Cooper, Thomas Scanlon, and Richard de Visser. 2016. “Perceived Barriers to Accessing Mental Health Services among Black and Minority Ethnic (BME) Communities: A Qualitative Study in Southeast England.” BMJ Open 6 (11): e012337. https://doi.org/10.1136/bmjopen-2016-012337.
“GAIN Diaspora African Communities in Nottingham Research – 2018”. 2018. GAIN.